Image by Freepik
Bone health is one of the realms where I think most people work under the assumption of “health” being the absence of pathology, rather than taking a more positive lens. Bone is far from the inert, structural tissue than many think of it as - it is an exceptionally dynamic tissue, constantly changing and adapting to the signals it is receiving.
How Does Bone Change?
Wollf’s Law
Named after the German anatomist and surgeon Julius Wolff, who coined it, this law states, in effect, that bones will respond and adapt to the forces that they are subjected to.
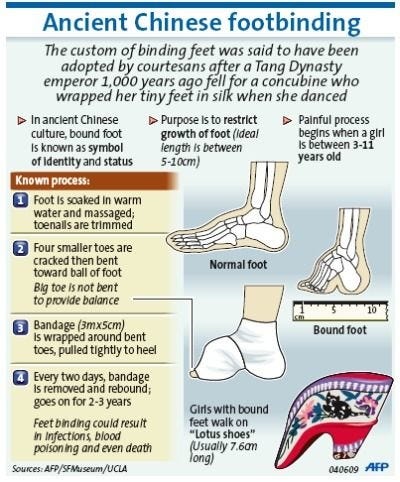
Perhaps the most intense example of this is ancient Chinese foot binding. I won’t go into the sociocultural factors here, but it is a perfect example of bones responding to forces imposed (and also why you should consider the shoes you wear - more on that in a footwear article upcoming)
Cells Involved
There are fundamentally two cell types that impact bone remodelling; osteoblasts which lay down new bone and osteoclasts which resorb bone.
This constant ebb and flow of laying down new bone and removing it acts akin to that of working with clay: add a little, trim away some to shape it etc.
But how do the cells know whether to build or resorb bone, in fact how does the body even know it has been loaded?
Enter “mechanotransduction,” where cells convert mechanical forces into biochemical signals (pretty cool right!?). The cells that do this in the case of bone are the primary bone cells; osteocytes.
This latin stuff is pretty logical really - osteo = bone, cytes=cells, blasts = building, clasts = resorbing.
Cool, so bones are loaded, osteocytes send biochemical messages and then the osteoblasts and osteoclasts do their thing. Great. So what?
What is Bone Health?
Bone health, likely has established definitions which are agreed upon by various organisations with acronyms. In this case though, and perhaps a useful working definition for people in the real world, I’d use a definition similar to the following:
Good bone health, is having high bone mineral density, with a high capacity to adapt to stresses imposed on the bone.
Now let’s break that down (see what I did there) to help us understand it better.
High bone mineral density (BMD) means that there has been enough bone loading - to stimulate the need for increase bone mineral density and enough nutrients and hormones to allow this to happen. Similarly, having an abundance or at least sufficient amounts of these hormones and nutrients is crucial for the ability to adapt to stresses imposed (it’s not enough to just have dense bone, you want to be able to adapt as necessary). To be honest, some may argue the latter is redundant given the former portion of this working definition and I’d listen but we won’t go there for now.
Nutrients and Hormones
We won’t spend too long here, the physiology swiftly becomes quite complex. To be overly simplistic, a lot of it (but not all of it) relates to calcium homeostasis in the body. Like many things in physiology, you’re looking for a “Goldilocks zone” with calcium as either too much or too little is a problem.
Hormones Involved in Bone Health:
Parathyroid hormone (PTH) - this works to increase calcium levels
Calcitonin - this works to decrease calcium levels
Oestrogen (we will get to menopause later) - low oestrogen can increase bone resorption
Thyroid hormones - these stimulate osteoblasts
Growth hormone- the net effect here is increased bone formation
Glucocorticoids - net result is increased bone resorption. Whilst we have these endogenously, we can also have the same result from prolonged use of corticosteroids too.
Nutrients Involved in Bone Health
Vitamin D - to be fair this is more like a hormone (we won’t get into it) but it is here due to it’s name. It plays a key role in calcium homeostasis.
Calcium - this shouldn’t surprise anyone, it is the key mineral in bones.
Protein - a key component of bone is actually protein.
Micronutrients - many other micronutrients are also important for bone health probably most notable vitamin K.
Carbohydrate and total energy - whilst a factor for everyone, this unlikely impacts non-athletes (more on this later).
What is Good Bone Mineral Density?
The way BMD it assessed is a little convoluted, but in short it compares people of the same age, biological sex and ethnicity. You are then placed into a percentile (osteopenia and osteoporosis are differing severities of low BMD based on this). So you can improve your bone mineral density compared to your relevant comparator group by losing less bone over time. This is because for most of our lives (beyond about 30 something years of age) we are losing BMD as you can see below.
From Santos et al
The significant, almost stepwise, drop in BMD in women is a representation of menopause, where oestrogen declines (see above requirements of hormones for bone health).
What are the Risks of Poor Bone Health?
As mentioned, osteopaenia and osteoporosis are on a spectrum (where osteoporosis is the more extreme end). Classification is with comparison to normative values from the reference population and low BMD (beyond these thresholds) will classify you as osteopaenic or, if more extreme, osteoporotic.
Whilst not healthy, and perhaps with their own consequences we have no discovered yet, these conditions are certainly manageable - I won’t touch on medications but there certainly are some. I will, however, touch on prevention aside from the nutrition and hormone health mentioned above. The real concern (in our current understanding) is falls and fractures. One challenge is healing of these, you know, because the bone isn’t good quality so it doesn’t heal well and surgery can be tricky because, you guessed it, the bone isn’t good quality.
Sounds horrible right? Good - we agree, it gets worse though.
Mortality rates post hip fracture are high, and yes generally fractured hips as a result of falls don’t happen in young healthy people but avoiding this should be a key goal. How high you ask? Numbers vary between studies and populations but 6 month mortality rates are ~ 13.5-25% and 12 month mortality rates are ~27-33% - you get the point, it’s not great. And that is just deaths, this doesn’t speak to impaired quality of life.
To make it worse still, bad enough osteoporosis means little force is needed for a fracture, and you can see fracture patterns which differ from those in people with good BMD. Specifically, compression fractures, which effectively result from gravity as the force acting on the bone.
You Mentioned Athletes, Energy and Carbohydrates
This is an area gaining steam in the public discourse, underfuelling as part of the risk for a host of problems related to Low Energy Availability (LEA) and Relative Energy Deficiency in Sport (RED-S). I briefly touched on these here, but in essence, prolonged mismatch between output and intake (so called LEA) can cause RED-S. RED-S is a syndrome with a host of issues, one of which is stress fractures. In fact, this portion of the syndrome is so prevalent that the earlier recognition of RED-S was as “the female athlete triad” the triad including low BMD. The update, acknowledging more wide ranging pathology as well as including the occurrence biological males, where the most classic first sign of issues is, you guessed it, a stress fracture. Interestingly though, the science continues to evolve and as mentioned before there are some early indications that there may be bone health issues (and broader RED-S risks) with low carbohydrate availability too, not just total caloric deficits, so watch this space.
Use it or Lose it
“Use it or lose it” is probably as close to a universal truth in physiology as we get. When it comes to bones - it’s called Wollf’s law (see above).
The most important thing you can do for BMD is to get it’s peak as high as possible, which requires tonnes of loading, food etc during childhood and through your 20s (that last bit no doubt caught some readers off guard - yeah we need to talk about declining exercise rates post high school but that’s for a different day).
If, as many readers would be, you’re beyond your mid 30’s it’s likely you’ve already achieved peak BMD (whatever that is for you) and it is time for the second most important thing you can do for your BMD - MAINTAIN IT!
Enter ‘use it or lose it’.
The problem here reminds me of a George Bernard Shaw quote:
“We don't stop playing because we grow old; we grow old because we stop playing.”
Hopefully you’ve joined the dots (and perhaps had a bit of a flashback of physical activity and exercise in the last decade or so) and are now thinking “I wonder if I am loading my bones enough”.
The Problem with Most of Our Bone Health Exercise Prescription
The bar is too low. We cannot keep looking at people as though they’re fragile and need to be wrapped in cotton wool. Exercise recommendations and even popular discourse around exercise (especially in those who’s age starts with a 5 or more) is often “low impact” - swimming, cycling, tai chi, yoga etc. Don’t get me wrong, these are all great forms of exercise (and the ones with balance components do help improve balance, which contributes to falls, though there are other ways to do this) but the low impact nature makes them low impact for bone health! Also, walking, despite all it’s benefits is not particularly helpful for increasing BMD.
So what should you do?
90’s hip hop is littered with the answer: Jump
Jumping is the easiest, cheapest, way to load your bones. Of course, the higher you jump the more force there is but estimates of ground reaction force (the force put into the ground) from jumping are 4.5x bodyweight. And yes, the runners reading this - that is also great for BMD. In fact, so is resistance training, though the magnitudes are less. The one area where resistance training may have the real edge is spinal loading (ie squats) to help with spinal BMD - thoracic spine ‘compression’ fractures are sadly quite common. This is because BMD improvements or maintenance are site specific - yes tennis players have different BMDs on their arms.
Given this and the fact that the most common fracture in general and an exceptionally common issue with falls is a wrist fracture (aka distal radius fracture) don’t forget to jump with your upper body too. Said less tongue in cheek - plyometrics (aka clap) pushups. Again, the height caveats exist here but the estimates are that these result in roughly 1.4x bodyweight forces. Of course these could be done without clapping, on knees (yes this is better than normal pushups due to loading rates) or other variations.
Note: talk with your healthcare/training team about including these and ramp them up slowly - something like a single jump/clap pushup of sub maximal intensity every 3 days and building up from there ESPECIALLY if you’re deconditioned.
Hopefully the importance of bone health is clear, as is the fact it should be something you’re thinking about already (regardless of age!). Likewise, hopefully this has empowered you to be able to make some very minor adjustments that will pay significant dividends later on - in ways you’ll never be able to quantify because avoiding a problem is unquantifiable and unknowable.
Happy jumping.
References
Rowe P, Koller A, Sharma S. Physiology, Bone Remodeling. [Updated 2023 Mar 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499863/
Santos L, Elliott-Sale KJ, Sale C. Exercise and bone health across the lifespan. Biogerontology. 2017 Dec;18(6):931-946. doi: 10.1007/s10522-017-9732-6. Epub 2017 Oct 20. PMID: 29052784; PMCID: PMC5684300.
Price CT, Langford JR, Liporace FA. Essential Nutrients for Bone Health and a Review of their Availability in the Average North American Diet. Open Orthop J. 2012;6:143-9. doi: 10.2174/1874325001206010143. Epub 2012 Apr 5. PMID: 22523525; PMCID: PMC3330619.
Fensham NC, Heikura IA, McKay AKA, Tee N, Ackerman KE, Burke LM. Short-Term Carbohydrate Restriction Impairs Bone Formation at Rest and During Prolonged Exercise to a Greater Degree than Low Energy Availability. J Bone Miner Res. 2022 Oct;37(10):1915-1925. doi: 10.1002/jbmr.4658. Epub 2022 Aug 10. PMID: 35869933; PMCID: PMC9804216.
Dayer SR, Mears SC, Pangle AK, Mendiratta P, Wei JY, Azhar G. Does Superior Bone Health Promote a Longer Lifespan? Geriatr Orthop Surg Rehabil. 2021 Aug 3;12:21514593211036231. doi: 10.1177/21514593211036231. PMID: 34395047; PMCID: PMC8358490.
Guzon-Illescas, O., Perez Fernandez, E., Crespí Villarias, N. et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res 14, 203 (2019). https://doi.org/10.1186/s13018-019-1226-6
Hannan EL, Magaziner J, Wang JJ, et al. Mortality and Locomotion 6 Months After Hospitalization for Hip Fracture: Risk Factors and Risk-Adjusted Hospital Outcomes. JAMA. 2001;285(21):2736–2742. doi:10.1001/jama.285.21.2736
Prodovic T, Ristic B, Rancic N, Bukumiric Z, Zeljko S, Ignjatovic-Ristic D. Factors Influencing The Six-Month Mortality Rate In Patients With A Hip Fracture: DEJAVNIKI, KI VPLIVAJO NA ŠESTMESEČNO STOPNJO UMRLJIVOSTI PRI BOLNIKIH Z ZLOMOM KOLKA. Zdr Varst. 2016 Feb 11;55(2):102-7. doi: 10.1515/sjph-2016-0015. PMID: 27284379; PMCID: PMC4845770.
Panula J, Pihlajamäki H, Mattila VM, Jaatinen P, Vahlberg T, Aarnio P, Kivelä SL. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord. 2011 May 20;12:105. doi: 10.1186/1471-2474-12-105. PMID: 21599967; PMCID: PMC3118151.
Paweł Szulc, Joshua R Lewis, Roland Chapurlat, Decline in muscle strength and physical function after fracture in men – the prospective STRAMBO study, Journal of Bone and Mineral Research, 2024;, zjae014, https://doi.org/10.1093/jbmr/zjae014
Mountjoy M, Ackerman KE, Bailey DM, et al. 2023 International Olympic Committee’s (IOC) consensus statement on Relative Energy Deficiency in Sport (REDs). Br J Sports Med 2023;57:1073–1097
Benedetti MG, Furlini G, Zati A, Letizia Mauro G. The Effectiveness of Physical Exercise on Bone Density in Osteoporotic Patients. Biomed Res Int. 2018 Dec 23;2018:4840531. doi: 10.1155/2018/4840531. PMID: 30671455; PMCID: PMC6323511.
Hu K, Cassimatis M, Girgis C. Exercise and Musculoskeletal Health in Men With Low Bone Mineral Density: A Systematic Review. Arch Rehabil Res Clin Transl. 2023 Dec 6;6(1):100313. doi: 10.1016/j.arrct.2023.100313. PMID: 38482104; PMCID: PMC10928274.
McNair PJ, Prapavessis H. Normative data of vertical ground reaction forces during landing from a jump. J Sci Med Sport. 1999 Mar;2(1):86-8. doi: 10.1016/s1440-2440(99)80187-x. PMID: 10331479.
Koch J, Riemann BL, Davies GJ. Ground reaction force patterns in plyometric push-ups. J Strength Cond Res. 2012 Aug;26(8):2220-7. doi: 10.1519/JSC.0b013e318239f867. PMID: 21986698.
Luokkala T, Laitinen MK, Hevonkorpi TP, Raittio L, Mattila VM, Launonen AP. Distal radius fractures in the elderly population. EFORT Open Rev. 2020 Jun 17;5(6):361-370. doi: 10.1302/2058-5241.5.190060. PMID: 32655892; PMCID: PMC7336190.
Sanchis-Moysi J, Dorado C, Olmedillas H, Serrano-Sanchez JA, Calbet JA. Bone and lean mass inter-arm asymmetries in young male tennis players depend on training frequency. Eur J Appl Physiol. 2010 Sep;110(1):83-90. doi: 10.1007/s00421-010-1470-2. Epub 2010 Apr 17. PMID: 20401491.