What to do When You've Slept Badly
What to for for health and performance when you've slept poorly
We have all been there, a bad night’s sleep and trying to pick up the pieces the next day. Yes, ideally we would sleep well but we also live in the real world. Unfortunately these nights of poor sleep often happen at inopportune times (when travelling for work, before important days etc). It is with this in mind that I thought folks would see value in this piece. If you do; please share it and/or comment below (or reply to the email).
What Happens When You Sleep Poorly?
I will preface this, with the fact that I think the health space specifically does a *should this be a positive or negative adjective? I can’t decide; but it’s a strong one* job of scaring people when it talks about these things. One could easily believe that they should be rushed to hospital after one instance of suboptimal circumstances. Don’t forget you are not a fragile organism, and you don’t need to chase perfection all the time.
With this as the caveat, it is worth explaining the consequences of a poor night’s sleep, partially to help nudge you to focus on your sleep if you aren’t already making it a top priority but more so to use this as a vessel to then explain the counter measures we can take to help remedy the situation.
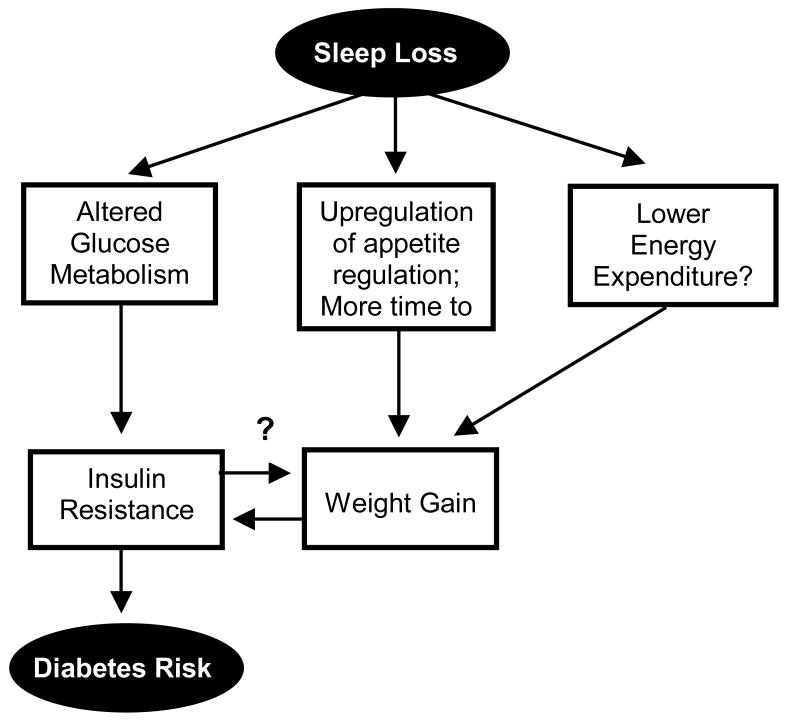
When we have had a poor night of sleep we suffer the consequences of a lack of recovery and our body trying to optimise things for the following day. The former means we have issues such as reduced beta amyloid clearance in the brain (a key player in Alzheimer’s) and the latter leads to a level of insulin resistance and increased hunger (via hunger hormones).
Actions to Take
There are some general actions that can be taken to help when you’ve not slept well which probably help any situation, before we discuss specific actions for health or performance.
Much of this won’t surprise many folks and may already be part of your strategy:
Nap - try to ensure this doesn’t create another issue for you on the second night, so try to keep it earlier rather than later in the day. For a real pickup, try a “caffeine nap”.
Movement - How much will vary based on goals (and what realm you are trying to perform in, if it is the sporting realm this becomes less important than say the boardroom), but this should definitely be part of your strategy and preferably be earlier in the day to aid in wakefulness and circadian rhythm reinforcement.
Creatine - given creatine’s ability to aid in brain energy and general cognitive function, it can be extremely helpful when sleep deprived.
Health
When it comes to managing the health consequences of sleep deprivation, we are really solving for a glucose dysregulation issue and thus the levers we can pull (aside from sleep) are largely around movement and nutrition.
The nutrition aspect of this metabolic situation is particularly important given the appetite and willpower changes that happen as a result of sleep deprivation. Appetite is increased, and evidence suggests we crave more calorie dense and processed foods, not to mention generally have lower willpower. As such one key factor in managing sleep deprivation is the removal of choice - don’t rely on willpower or choice, have some go to foods and meals that are high in protein and fibre to help manage the glucose dysregulation and increase satiety.
When it comes to movement, there are two factors to consider; physical activity and exercise (more on the difference here). Avoiding significant periods of inactivity is an excellent way to improve glucose metabolism, regardless of sleep status (or whether you have diabetes or not).
With respect to exercise specifically, research supports the use of higher intensity exercise specifically HIIT type activity. (*I have a feeling this is because the glycaemic impact of exercise is a product of intensity & duration and thus the duration of lower intensity exercise required is large - so the effects are easier to see in research and for most people higher intensity would be preferable.) Ideally this exercise should be done earlier in the day, to have its insulin sensitising and glucose regulating effects impact the day of interest.
Performance
Anecdotally many athletes (including ‘boardroom athletes’) would agree, sleeping well the night prior to a big competition is difficult and often performance following a single night of poor sleep is certainly possible. This is probably a result the the hormonal milieu which results from the pressure of competition (this is a good thing) - in fact, this very phenomenon was why many Eastern Bloc coaches delineated competition and training maximums in strength athletes (something I think endurance athletes would do well to think about).
This likely extends to non-athletic performance too. Again, many folks would remember performing fairly well on exams despite a suboptimal night’s sleep prior to the exam.
This is not to encourage sleep deprivation, but the impact of the belief that this would be a barrier is significant. In fact some interesting research has been done suggesting that a nocebo (a negative placebo) type effect exists where belief one has had poor sleep may impair their performance (more on this below when discussing wearables).
Despite all of this, one may decide to take some action and if so, in addition to the above suggestions; coffee/caffeine is your friend - again, be a little careful on timing here (as usual) given caffeine can cause a knock on effect if you have it too late in the day. That said, it is accepted as one of the best (legal) performance enhancers available, regardless of sleep status but clear in light of sleep deprivation it has another potential upside.
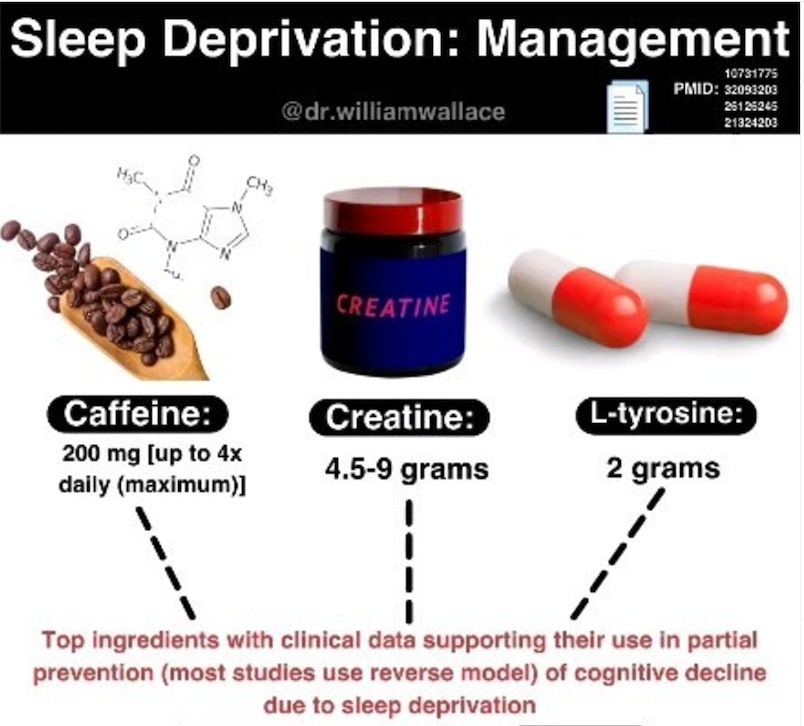
Cognitive Performance Stack For Sleep Deprivation
Hat tip to Dr William Wallace on this stack, it’s something I have been using and find to be helpful (though it would be hard to be sure it is working - using the lenses I often discuss, it’s low risk and downside in my mind so why not).
It is worth noting that more recently, a higher (0.35 g/kg) dose of creatine has been advocated in sleep deprivation (this is closer to 20-30g than 9g for most adults).
Some Potential Sleep Aids
I have been pretty clear in the fact that there is a potential for a knock on effect of a night’s bad sleep. That is, our efforts to mitigate this bad night’s sleep, may mean we create a second bad night of sleep and, at least in my mind, this is the last thing someone should do (perhaps with the exception of a single day performance).
Similarly, it is worth considering making extra effort to aid in sleep the second night to get back on track so to speak. Some strategies include:
Glycine - an amino acid with interesting potential for sleep enhancement.
Exercise - as mentioned above this has other benefits in the context of sleep deprivation but exercise improves sleep significantly. That said, exercising earlier in the day or at lower intensity if in the evening is better in this context as higher intensity exercise late at night can impair sleep.
Light - the basics of sleep and circadian rhythm revolve around light; exposing yourself to light, preferably sunlight earlier in the day, can aid in circadian rhythm reinforcement and sleep.
Sleep Hygiene - as discussed in this article, sleep hygiene is key to good sleep. This includes a wind down routine, sleeping environment and alcohol avoidance.
Magnesium - interestingly literature is not particularly supportive of the benefit of magnesium in sleep (this is may be due to challenges in researching a topic like this) but anecdotally many people see great benefits. Given it’s importance in metabolism and the low risk and downside it may be worth trying for people (more on the calculus of decisions like this here).
Other Considerations
Whether anticipating a bad night’s sleep given the circumstances, or dealing with an unforeseen bad night’s sleep, it may be pertinent to make some adjustments as a result.
Of course, building a nap into the day is something already mentioned, but if you know a bad night’s sleep is coming, ‘banking some sleep’ with a nap ahead of the potentially bad night could be helpful. Again, it is important to do this far away enough from the night to prevent it exacerbating the problem.
In a similar vein, it may be worth engineering your day to reinforce circadian rhythms. This can help by prevent the knock on effect to a second poor night’s sleep and potentially increasing alertness after a bad night’s sleep. For more on this, the principles in this article may help.
Finally, it may be worth ditching your sleep tracker for a night or two. As mentioned, the negative impact of this data can be real (even if you have slept well and it’s sham data!). Some folks opt out of tracking their data in this case, and that’s not an unreasonable choice. For many this means travelling without a tracker (and thus a charger - so maybe it’s a good call!) because we know travel will often impair sleep. Good trackers may even let you track and blind yourself to the data if needed - something athletes are well served doing on competition day (boardroom athletes too). It would be nice to see this built in to more trackers, that’s for sure (the bill is in the mail guys) - the world’s best cyclist actually gets his girlfriend to check his so he doesn’t have to when perfoming. Until this is the case though, the choice to track sleep on nights when bad sleep is coming (or has occurred) largely boils down to personality and how much you can detach from the data as an interesting piece of information rather than deterministic.
Summary
The actions taken in the context of a bad night’s depend in part of goals. Some behaviours such as napping will likely help any outcome, but other such as dietary modification are best served in specific contexts. Caffeine is likely your friend when it comes to performance but you probably already knew this. It’s certainly worth considering optimising for avoidance of a second bad night of sleep and engineering your day as such.
Whilst not condoning sleeping poorly (it’s something I personally work exceptionally hard to avoid), it is a reality and hopefully this helps with the reality of this for readers.
References
Shokri-Kojori E, Wang GJ, Wiers CE, Demiral SB, Guo M, Kim SW, Lindgren E, Ramirez V, Zehra A, Freeman C, Miller G, Manza P, Srivastava T, De Santi S, Tomasi D, Benveniste H, Volkow ND. β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proc Natl Acad Sci USA. 2018 Apr 9. pii: 201721694. doi: 10.1073/pnas.1721694115. [Epub ahead of print] PMID: 29632177.
Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007 Jun;11(3):163-78. doi: 10.1016/j.smrv.2007.01.002. Epub 2007 Apr 17. PMID: 17442599; PMCID: PMC1991337.
Sharma S, Kavuru M. Sleep and metabolism: an overview. Int J Endocrinol. 2010;2010:270832. doi: 10.1155/2010/270832. Epub 2010 Aug 2. PMID: 20811596; PMCID: PMC2929498.
Rogers EM, Banks NF, Jenkins NDM. The effects of sleep disruption on metabolism, hunger, and satiety, and the influence of psychosocial stress and exercise: a narrative review. Diabetes Metab Res Rev. 2024;e3667. https://doi.org/10.1002/dmrr.3667
Centofanti S, Banks S, Coussens S, Gray D, Munro E, Nielsen J, Dorrian J. A pilot study investigating the impact of a caffeine-nap on alertness during a simulated night shift. Chronobiol Int. 2020 Sep-Oct;37(9-10):1469-1473. doi: 10.1080/07420528.2020.1804922. Epub 2020 Aug 20. PMID: 32819191.
Horne JA, Reyner LA. Counteracting driver sleepiness: effects of napping, caffeine, and placebo. Psychophysiology. 1996 May;33(3):306-9. doi: 10.1111/j.1469-8986.1996.tb00428.x. PMID: 8936399.
Horne JA, Reyner LA. Counteracting driver sleepiness: effects of napping, caffeine, and placebo. Psychophysiology. 1996 May;33(3):306-9. doi: 10.1111/j.1469-8986.1996.tb00428.x. PMID: 8936399.
Bonnet MH, Arand DL. The use of prophylactic naps and caffeine to maintain performance during a continuous operation. Ergonomics. 1994 Jun;37(6):1009-20. doi: 10.1080/00140139408963714. PMID: 8026448.
Gordji-Nejad, A., Matusch, A., Kleedörfer, S. et al. Single dose creatine improves cognitive performance and induces changes in cerebral high energy phosphates during sleep deprivation. Sci Rep 14, 4937 (2024). https://doi.org/10.1038/s41598-024-54249-9
Surabhi Bhutani, James D Howard, Rachel Reynolds, Phyllis C Zee, Jay Gottfried, Thorsten Kahnt. Olfactory connectivity mediates sleep-dependent food choices in humans. eLife, 2019; 8 DOI: 10.7554/eLife.49053
El Fatouhi D, Héritier H, Allémann C, Malisoux L, Laouali N, Riveline JP, Salathé M, Fagherazzi G. Associations Between Device-Measured Physical Activity and Glycemic Control and Variability Indices Under Free-Living Conditions. Diabetes Technol Ther. 2022 Mar;24(3):167-177. doi: 10.1089/dia.2021.0294. Epub 2021 Dec 14. PMID: 34648353; PMCID: PMC8971971.
Qiu, S., Cai, X., Chen, X. et al. Step counter use in type 2 diabetes: a meta-analysis of randomized controlled trials. BMC Med 12, 36 (2014). https://doi.org/10.1186/1741-7015-12-36
Nicholas J. Saner, Matthew J-C. Lee, Jujiao Kuang, Nathan W. Pitchford, Gregory D. Roach, Andrew Garnham, Amanda J. Genders, Tanner Stokes, Elizabeth A. Schroder, Zhiguang Huo, Karyn A. Esser, Stuart M. Phillips, David J. Bishop, Jonathan D. Bartlett, Exercise mitigates sleep-loss-induced changes in glucose tolerance, mitochondrial function, sarcoplasmic protein synthesis, and diurnal rhythms, Molecular Metabolism, Volume 43, 2021, 101110, ISSN 2212-8778, https://doi.org/10.1016/j.molmet.2020.101110.
Trabelsi K, BaHammam AS, Chtourou H, Jahrami H, Vitiello MV. The good, the bad, and the ugly of consumer sleep technologies use among athletes: A call for action. J Sport Health Sci. 2023 Jul;12(4):486-488. doi: 10.1016/j.jshs.2023.02.005. Epub 2023 Mar 1. PMID: 36868375; PMCID: PMC10362482.
Draganich C, Erdal K. Placebo sleep affects cognitive functioning. J Exp Psychol Learn Mem Cogn. 2014 May;40(3):857-64. doi: 10.1037/a0035546. Epub 2014 Jan 13. PMID: 24417326.
Tsai YS, Chen TT, Chan YC, Huang CC, Lai TF, Liao Y, Metcalfe RS, Chen YC, Wang HS. Acute caffeine supplementation offsets the impairment in 10-km running performance following one night of partial sleep deprivation: a randomized controlled crossover trial. Eur J Appl Physiol. 2024 Oct 22. doi: 10.1007/s00421-024-05638-5. Epub ahead of print. PMID: 39438312.
Axelsson J, Vyazovskiy VV. Banking Sleep and Biological Sleep Need. Sleep. 2015 Dec 1;38(12):1843-5. doi: 10.5665/sleep.5222. PMID: 26564136; PMCID: PMC4667377.
Pomeroy DE, Tooley KL, Probert B, Wilson A, Kemps E. A Systematic Review of the Effect of Dietary Supplements on Cognitive Performance in Healthy Young Adults and Military Personnel. Nutrients. 2020 Feb 20;12(2):545. doi: 10.3390/nu12020545. PMID: 32093203; PMCID: PMC7071459.
Reyner LA, Horne JA. Early morning driver sleepiness: effectiveness of 200 mg caffeine. Psychophysiology. 2000 Mar;37(2):251-6. PMID: 10731775.
Attipoe S, Zeno SA, Lee C, Crawford C, Khorsan R, Walter AR, Deuster PA. Tyrosine for Mitigating Stress and Enhancing Performance in Healthy Adult Humans, a Rapid Evidence Assessment of the Literature. Mil Med. 2015 Jul;180(7):754-65. doi: 10.7205/MILMED-D-14-00594. PMID: 26126245.
Cook CJ, Crewther BT, Kilduff LP, Drawer S, Gaviglio CM. Skill execution and sleep deprivation: effects of acute caffeine or creatine supplementation - a randomized placebo-controlled trial. J Int Soc Sports Nutr. 2011 Feb 16;8:2. doi: 10.1186/1550-2783-8-2. PMID: 21324203; PMCID: PMC3049131.
Gordji-Nejad, A., Matusch, A., Kleedörfer, S. et al. Single dose creatine improves cognitive performance and induces changes in cerebral high energy phosphates during sleep deprivation. Sci Rep 14, 4937 (2024). https://doi.org/10.1038/s41598-024-54249-9